 Abraham Lincoln
If given the truth, the people can be depended upon to meet any national crisis...
Abraham Lincoln
If given the truth, the people can be depended upon to meet any national crisis...
 Guildford news...
for Guildford people, brought to you by Guildford reporters - Guildford's own news service
Guildford news...
for Guildford people, brought to you by Guildford reporters - Guildford's own news service
A Third of Ambulance Call Outs To Be Handled Remotely
Published on: 9 Apr, 2024
Updated on: 10 Apr, 2024
By Emily Dalton
local democracy reporter
Over a third of South East Coast Ambulance (SECAmb) service responses will in future be done remotely, over the telephone or by virtual online consultation, under a new five-year strategy.
At a board meeting last week (April 4) the NHS Trust said that as it prepares for a 15 per cent increase in patient demand over the next five years its current care model is no longer “fit for purpose”. Increasing demands on the service include the increased complexity of health care, an ageing population and changing areas of deprivation.
By 2029, the Trust is aiming to signpost over a third of all its patients to another service, leaving only 65 per cent of patients with an ambulance response. The change will affect Surrey, Thames Valley, Kent and Medway as well as Sussex Integrated Care Systems (ICS).
Simon Weldon, CEO, gave a reassurance that SECAmb would still be there to protect and look after the sick who needed an ambulance. He added: “If patients don’t need an ambulance, we can help you get you to a place which can meet your healthcare needs.”
Urgent medical needs such as cardiac arrest, a stroke, heart attack, pneumonia, childbirth and newborn care would still be attended to by ambulances, the Trust said.
Delivering this strategy over the next three years, SECAmb expects it to meet emergency care needs within the national standards of 7 minutes for calls for immediate life-threatening and time-critical injuries and illnesses; and 18 minutes for emergency calls.
For non-emergency patients, virtual care will be provided via an assessment by a remote senior clinician. Meeting documents said this would enable patients to be “cared for directly or referred to the most appropriate care provider”.
Investing in a data and digital strategy was highlighted as a key part of the new direction. The board heard how new technology like AI would help the SECAmb make better decisions and lead virtual consultations. These could be used to respond to patient needs in a remote and professional setting rather than sending an ambulance.
Meeting documents revealed that 88 per cent of patients received an ambulance response; but a SECAmb officer said the outcomes from the cases indicated only 31 per cent of patients needed clinical care.
Only 12 per cent of patients are currently referred or signposted to another service rather than receiving ambulance care; but under the new strategy for 2029, this will increase to 35 per cent target.
Team member for SECAmb Matt Dechaine said: “Sending a fully kitted ambulance is a very expensive way for the public purse to respond to patient needs, when other services may be able to address it in a cost-effective way.”
Covering five years, the new strategy will be carried out in three phases: designing new models of care, collaborating with partners and developing a digital strategy; implementing the change and finalising and improving the operational model. Digitalisation of the service will begin in phase 2, with electronic health records deployed by March 2025.
SECamb identified its current model as “unsustainable when challenged” from an operational, workforce and financial perspective. The Trust found it would need to employ 600 more people over the next five years to respond to demand.
Not all non-emergency patient consultations will be resolved solely over the telephone. Simon Weldon told the board that the strategy aims to “align patient needs with ambulance services”.
Over 2,000 staff, 400 volunteers and 350 members of the public have been consulted on the strategy, with the Trust saying it has been “clinically led”. System partners have also been invited to 20 sessions to share their views.
The full new SECAmb strategy is set to be published in May 2024.
Responses to A Third of Ambulance Call Outs To Be Handled Remotely
Leave a Comment Cancel reply
Please see our comments policy. All comments are moderated and may take time to appear. Full names, or at least initial and surname, must be given.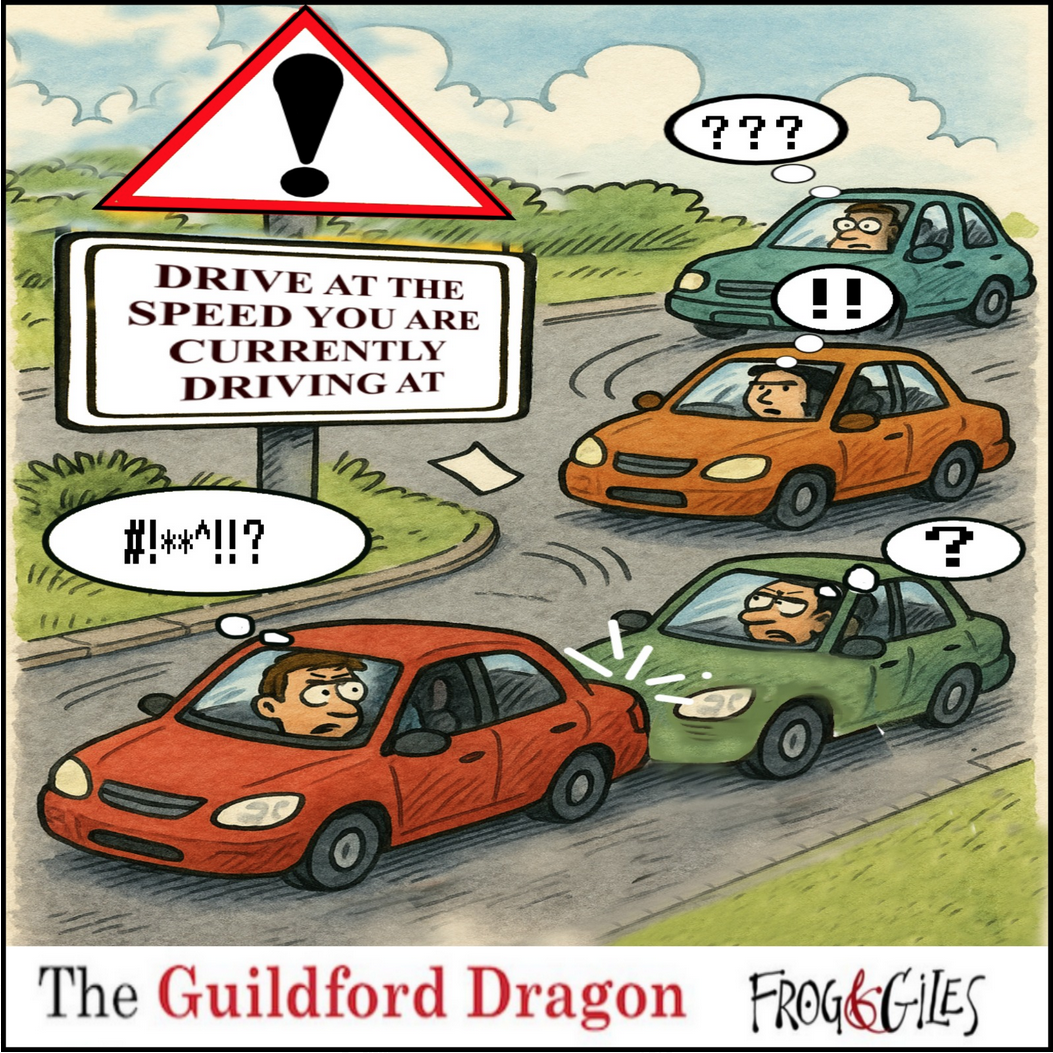
Click on cartoon for Dragon story: Public Asked for Views on SCC’s Proposal for Reduced Speed Limits

Recent Articles
- Driver Given Suspended Sentence After Serious Collision With Motorcycle
- Birdwatcher’s Diary No.329
- Opinion: We Must Plan To Deal with Guildford Gridlock
- A281 Closure – Further Delay to Re-opening
- Centenary of Wood Street’s First Place of Worship, my Baptism Link with It and the Revd Deedes and his Family
- Care For Guildford Asks: Could You Be One Of Our Volunteers?
- Flashback: There Are Lessons To Learn from the Juneja Case – The Council Must Admit It
- GBC’s Plan For a Thriving Guildford ‘Is Our Promise to Residents’ Says Council Leader
- Highways Bulletin: Campaign for Better Transport
- Check on Forgetful Neighbours During Hot Weather Urges Alzheimer’s Society


Recent Comments
- Nigel Base on Letter: Recreational Rowing Might Be the Answer
- Caroline Turnbull on Letter: Recreational Rowing Might Be the Answer
- Caroline Freeman on Letter: Recreational Rowing Might Be the Answer
- David Roberts on Letter: Recreational Rowing Might Be the Answer
- Tony Harrision on A281 Closure – Further Delay to Re-opening
- Valerie Thompson on Royal Surrey Patients Complain Changes Won’t Fix Underlying Parking Problem
Search in Site
Media Gallery
Dragon Interview: Local Artist Leaves Her Mark At One of England’s Most Historic Buildings
January 21, 2023 / No Comment / Read MoreDragon Interview: Lib Dem Planning Chair: ‘Current Policy Doesn’t Work for Local People’
January 19, 2023 / No Comment / Read MoreA3 Tunnel in Guildford ‘Necessary’ for New Homes, Says Guildford’s MP
January 10, 2023 / No Comment / Read More‘Madness’ for London Road Scheme to Go Ahead Against ‘Huge Opposition’, Says SCC Leader
January 6, 2023 / No Comment / Read MoreCouncillor’s Son Starts Campaign for More Consultation on North Street Plan
December 30, 2022 / No Comment / Read MoreCounty Council Climbs Down Over London Road Works – Further ‘Engagement’ Period Announced
December 14, 2022 / No Comment / Read MoreDragon Interview: GBC Reaction to the Government’s Expected Decision to Relax Housing Targets
December 7, 2022 / No Comment / Read MoreHow Can Our Town Centre Businesses Recover? Watch the Shop Front Debate
May 18, 2020 / No Comment / Read More









Mark Stamp
April 10, 2024 at 6:13 pm
I don’t disagree that there are ambulance call outs that could be handled in other ways but are probably happening because people are not able to get the treatment they need already.
I presume that the other healthcare providers that those in need of care will be directed towards will be A&E, GPs and local pharmacies all of which have their own pressures. Who is responsible for ensuring that there is an integrated plan rather than the various trusts each having their own plan to save money but risking people in need falling through the cracks?
Much more focus needs to be put on improving health to reduce people getting sick in the first place, for example insulating homes so people aren’t living in damp and drafty properties.