 Abraham Lincoln
If given the truth, the people can be depended upon to meet any national crisis...
Abraham Lincoln
If given the truth, the people can be depended upon to meet any national crisis...
 Guildford news...
for Guildford people, brought to you by Guildford reporters - Guildford's own news service
Guildford news...
for Guildford people, brought to you by Guildford reporters - Guildford's own news service
Letter: My Different Experiences at the Royal Surrey
Published on: 8 Aug, 2023
Updated on: 8 Aug, 2023
From: Paul Robinson
In response to: Dragon Interview – The Royal Surrey’s CEO, Louise Stead
After 35 years of having private medical cover provided by my employer, it is only since I retired three years ago that I have had to use NHS second-line medical care at the Royal Surrey.
My first experience was about a year after retirement when I was diagnosed with prostate cancer and I cannot praise enough the speed at which I was treated and the level of care I received at the Stokes Centre.
Once I had received a higher-than-normal PSA result, within a week I had an MRI scan which didn’t show anything up. But a subsequent biopsy confirmed cancer was present. I was treated within three months and so far the results have been successful.
In late June this year, I had to go into the Short Stay Surgical Unit for some day case surgery. My experience could not have been more different.
I checked in at 7.30am, as requested, but I as there were no beds available I had to sit around in the waiting area until about 10 o’clock when I was taken down to be prepped for surgery.
During that time I had the usual chats with the surgeon and the anaesthetist. For these conversations I was taken to side rooms which were actually small store rooms! One of the staff actually called them “broom cupboards”.
At about 10 o’clock I was taken away to be prepared for surgery and was once again taken to a store room to change into a gown and then walked to theatre.
After surgery, I was kept in the recovery room for about three hours until a ward bed became available. Apart from being given a cup of tea and a sandwich I didn’t see any nursing staff unless I buzzed them.
The surgeon saw me after about an hour of being put in the ward and said I could go home after I had urinated. After I had I went back to my bed and buzzed the nurse to tell her I had been to the toilet but while in the bathroom I had come over very hot and weak-kneed. She just looked at me as if to say, “What are you telling me this for?”
I had to explain what the surgeon had said about going home. I also expected some rudimentary health checks after reporting how I had felt in the bathroom or to be told that they were quite common side effects after surgery, but she said nothing.
At about 5 o’clock another patient was given his evening meal so I thought I had better see if I was now staying the night. I called a student nurse over and asked what the game plan was for me.
She said I was going home, but there had been no indication of that since my bathroom visit, until I asked. Within about 20 minutes of asking I was given my discharge paper and medication.
The only plus points of this experience were how attentive the recovery room staff were and apologetic for the wait for a ward bed.
I had waited four months between initial consultation and the procedure, which I thought was very reasonable considering the industrial action and the Covid backlog. I was expecting a wait of over a year.
I fed back my experience to the hospital and, within a few hours, a matron rang me back to talk to me about it. Although they couldn’t identify the nurse involved she said it would be mentioned at team briefings.
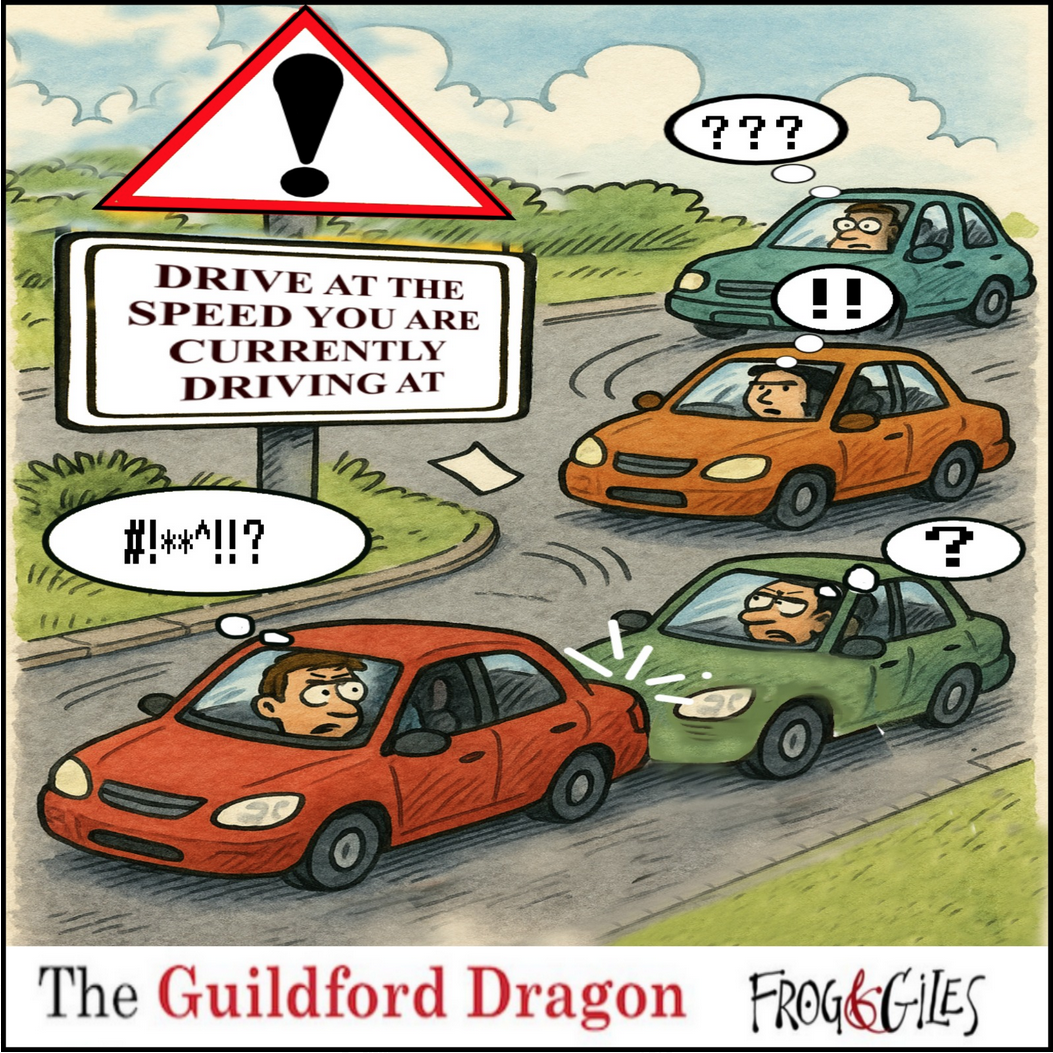
Click on cartoon for Dragon story: Public Asked for Views on SCC’s Proposal for Reduced Speed Limits

Recent Articles
- Volunteers Are Needed To Test My Wearable Wellbeing Technology
- Mayor’s Diary: May 23 – June 8
- Work to Repair Cottage on Closed A281 Underway
- Letter: Not All PIP Claimants Need It
- AI Technology at the Forefront of Surrey Conservation Project
- Mayor of Guildford Drops In on One of His Chosen Charities
- The Church’s Message Is As Relevant As Ever, Says Ash’s Retiring Priest
- CANCELLED: Have a Blooming Picnic – June 7
- Eight Out of Ten PIP Claimants in Guildford Face Cuts to Their “Lifeline”
- Waverley’s New Discretionary CIL Review Scheme To Be Revealed Soon


Search in Site
Media Gallery
Dragon Interview: Local Artist Leaves Her Mark At One of England’s Most Historic Buildings
January 21, 2023 / No Comment / Read MoreDragon Interview: Lib Dem Planning Chair: ‘Current Policy Doesn’t Work for Local People’
January 19, 2023 / No Comment / Read MoreA3 Tunnel in Guildford ‘Necessary’ for New Homes, Says Guildford’s MP
January 10, 2023 / No Comment / Read More‘Madness’ for London Road Scheme to Go Ahead Against ‘Huge Opposition’, Says SCC Leader
January 6, 2023 / No Comment / Read MoreCouncillor’s Son Starts Campaign for More Consultation on North Street Plan
December 30, 2022 / No Comment / Read MoreCounty Council Climbs Down Over London Road Works – Further ‘Engagement’ Period Announced
December 14, 2022 / No Comment / Read MoreDragon Interview: GBC Reaction to the Government’s Expected Decision to Relax Housing Targets
December 7, 2022 / No Comment / Read MoreHow Can Our Town Centre Businesses Recover? Watch the Shop Front Debate
May 18, 2020 / No Comment / Read More







Recent Comments